Acne Nodulocystica (Nodular acne)
Medically reviewed by The Dermatologists and written by Dr. Alexander Börve
- Affected Groups: Nodulocystic acne predominantly affects adolescents and young adults, with a higher incidence in males. It’s associated with genetic predispositions and environmental factors like diet and certain medications.
- Causes: The development is multifactorial, involving increased sebaceous gland activity, abnormal follicle keratinization, bacterial growth, and inflammation.
- Symptoms: Characterized by deep, painful nodules and cysts on the face and upper trunk, which can lead to significant scarring.
- Diagnosis: Primarily clinical, with the potential for hormone tests if systemic symptoms suggest an underlying condition.
- Treatment: Oral isotretinoin is the cornerstone of treatment, aimed at preventing scarring. Other options include intralesional steroids for persistent lesions and, in severe cases, antibiotics or immunomodulators.
Nodular acne is a challenging condition that goes beyond the surface, affecting deeper layers of the skin and often resulting in significant discomfort and scarring.
What is Nodular Acne?
Nodular acne is a severe form of acne vulgaris characterized by the development of large, painful, and inflamed nodules beneath the surface of the skin. These nodules are deeper and more substantial than typical pimples, often extending deep into the layers of the dermis. A ‘nodule’ is described as a firm skin mass or thickening measuring at least 5 mm in diameter, which can appear on various areas of the body, including the face, chest, and back.[1]
The development process of nodular acne begins with the clogging of hair follicles by excess oil (sebum) and dead skin cells. This blockage creates an ideal environment for the proliferation of bacteria, particularly Propionibacterium acnes. As these bacteria multiply, they trigger inflammation and immune responses within the skin, leading to the formation of nodules.[2] The inflammation extends deep into the surrounding tissues, resulting in the characteristic painful and tender nature of nodular acne lesions.
How to Identify Nodular Acne
Unlike surface level pimples, nodular acne will be deep seated painful bumps that can be tender to touch. According to the Investigator’s Static Global Assessment scale, severe nodular acne is classified as grade 4 or 5 acne, presenting with pronounced redness, inflammation, nodules, cysts, and scarring.[3] Inflammation gives rise to the characteristic features, redness, pain and tenderness.

Symptoms of nodular acne, including red slightly raised spots (papules), pus-filled spots (pustules), and deeper inflamed cysts that may be painful
Khammari A. et al. conducted a study in 2019 to observe and document the evolution of the nodules in nodular acne and reports that the evolution takes place in one of two ways. Nodules progressed into papules and subsequently into atrophic scars occur in 37.9% of cases, while 31.8% of nodules directly progressed into atrophic scars.[1] Complete clearance was observed only in 11.4% of the cases. Therefore, if you have nodular acne, you will almost invariably be able to find dark coloured rough scars on your skin, as the result of the regressed nodule with time. They also found that the longer you have nodular acne, the more chances of the nodules turning into scars rather than completely clearing away.[1]

Nodular acne scarring, indicating previous acne lesions’ healing and tissue damage
Furthermore, nodular acne does not typically develop a visible white or black “head” like other types of acne, as inflammation occurs deep within the skin. Also, they do not progress or heal as rapidly as other types of acne do. On average, it takes about 4 weeks for a nodule to fully resolve or turn into a scar.[1]
Additionally, nodular acne may advance to affect not only specific areas but also spread across the entire face, chest, and back.

Nodular acne on the back
In certain instances, these lesions may merge, forming sinus tracts, and in severe cases, they can involve the entire face, leading to a condition known as acne conglobata.[4]
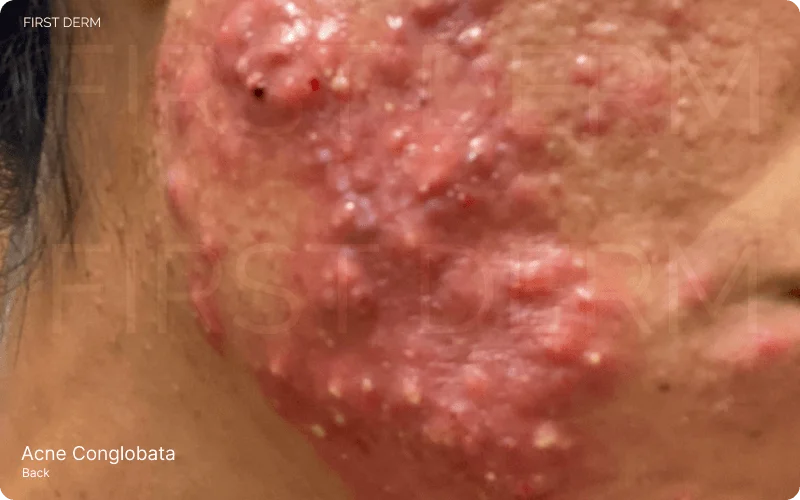
Severe Acne Conglobata: A complex condition characterized by cystic nodules, deep abscesses, and connecting sinus tracts, showcasing the extensive and inflammatory nature of this acne variant

Nodular vs. Cystic Acne

Comparison image showing two types of severe acne: On the left, nodular acne with red slightly raised spots (papules) and pus-filled spots (pustules); on the right, cystic acne characterized by a single, reddish, slightly raised cyst
Nodular acne presents as solid, painful lesions beneath the skin, while cystic acne forms fluid-filled sacs which may look yellowish due to the pus accumulated within. Also, these cysts are often softer and more fluctuant than nodules. Though similar in severity, they differ in texture and appearance. Both can be painful, lead to scarring and require professional treatment. Their common features often lead to confusion, emphasizing the importance of accurate diagnosis for effective management.
Treatment Options for Nodular Acne
It is very important to consult a medical professional when it comes to nodular acne because unless it receives aggressive and effective treatment at an early stage, there is a high risk of progressing into more severe and chronic forms.[3] Treatment options for nodular acne encompass various approaches mostly depending on the severity of the condition and the individual’s needs. Also, a combination of medication is always preferred in order to prevent antimicrobial resistance, which is an emerging problem worldwide.[5]
Oral medication
Unlike the less severe forms of acne where the first line treatment is topical retinoids combined with an antibiotic agent, in nodular acne, the first and best option is oral isotretinoin.[3]
For many years, oral antibiotics, mainly tetracyclines, have been the initial treatment choice for severe nodular acne, often resistant to other therapies.[3] However, due to worries about adverse effects, patient compliance, and antibiotic resistance, researchers sought alternative treatments and combinations to address the complex causes of the condition. Isotretinoin, an oral retinoid introduced in 1982, has emerged as the preferred therapy for severe acne, transforming its treatment landscape.[3] However, isotretinoin is not safe to be used in pregnancy because of its teratogenic effects.[5]
Oral antibiotics such as tetracycline, doxycycline, oxytetracycline, minocycline and erythromycin are used for people who are contraindicated for isotretinoin therapy.[3] It is very important to keep in mind that antibiotics are not recommended for a period of more than 4 to 5 months due to the rising antibiotic resistance.[6]
Topical Medications
Your dermatologist may prescribe topical creams, gels, or solutions containing ingredients like retinoids, benzoyl peroxide, or topical antibiotics that target localized lesions, reducing inflammation and preventing new breakouts.[3] The duration of treatment depends on how severe the acne is, and the way it responds to the treatment. Benzoyl peroxide is a commonly used nonantibiotic cream that shows complimentary action when used together with topical retinoids or topical antibiotics. This helps to minimize antibiotic resistance.
Hormonal Therapy
Hormonal therapy, including oral contraceptives and spironolactone, is used in women with various hormonal imbalances, such as polycystic ovarian syndrome. These agents reduce androgens, improving acne after 2–4 months of treatment.[3]
Corticosteroids
Low-dose oral corticosteroids can effectively treat acne related to adrenal hormone excess. They suppress excess androgen production. Low dose prednisolone or dexamethasone are such corticosteroids which can be especially helpful in managing severe flares of acne.[3]
Other procedures
There are some office-based treatments your dermatologist may offer, which are targeted approaches to address specific concerns associated with nodular acne. One such method is intralesional corticosteroid injections, which rapidly reduce inflammation and pain associated with individual nodules.[3] Additionally, adjunctive procedures such as chemical peels, light laser therapy and photodynamic therapy may help improve overall skin texture and reduce the appearance of acne scars.[7]
To summarize, the treatment modalities suggested by the global alliance for Nodular Acne look like this.[8]
First choice: oral isotretinoin
Second choice: oral antibacterial agent + topical retinoid + benzoyl peroxide
Alternatives: Oral spironolactone and/or oral contraceptive + topical retinoid ± benzoyl peroxide
Adjuncts: Oral corticosteroids
Office procedures: intralesional corticosteroid injections, chemical peels, light laser therapy and photodynamic therapy
Additional Tips for Better Results
For preventing nodular acne and maintaining skin health, adhere to basic skincare practices: cleanse gently twice daily, moisturize with non-comedogenic products, and apply sunscreen daily. Avoid harsh products and refrain from picking at acne lesions. Adopt a healthy lifestyle with a balanced diet and stress management. If nodular acne persists or worsens, consult a dermatologist promptly. Professional intervention can offer tailored treatment options, prevent scarring, manage severe cases effectively and help minimize psychological burden associated. Early dermatological care not only addresses current concerns but also reduces the likelihood of acne recurrence, promoting long-term skin health and confidence.
Please note: The treatment options discussed in this article for nodular acne are provided for informational purposes only and should not be considered as medical advice. It is important to consult with a dermatologist or healthcare professional to receive a diagnosis and personalized treatment plan, as treatments may vary based on individual conditions and health profiles. Always seek the guidance of a qualified healthcare provider with any questions you may have regarding a medical condition.
Source
- Khammari A, Blanchet-Réthoré S, Bourdès V, Marty C, Piketty C, Dréno B. Evolution and duration of nodules in severe nodular acne on the back: results from a four-week non-interventional, prospective study. J Eur Acad Dermatol Venereol. 2019;33(3):601-607. doi:10.1111/jdv.15407
- Tanghetti EA. The role of inflammation in the pathology of acne. J Clin Aesthet Dermatol. 2013 Sep;6(9):27-35. PMID: 24062871; PMCID: PMC3780801.
- Newman MD, Bowe WP, Heughebaert C, Shalita AR. Therapeutic considerations for severe nodular acne. Am J Clin Dermatol. 2011;12(1):7-14. doi:10.2165/11532280-000000000-00000
- Shalita AR. Acne: clinical presentations. Clin Dermatol. 2004;22(5):385-386. doi:10.1016/j.clindermatol.2004.03.012
- López-Estebaranz JL, Herranz-Pinto P, Dréno B; el grupo de dermatólogos expertos en acné. Consensus-Based Acne Classification System and Treatment Algorithm for Spain. Consenso español para establecer una clasificación y un algoritmo de tratamiento del acné. Actas Dermosifiliogr. 2017;108(2):120-131. doi:10.1016/j.ad.2016.10.001
- How long can I take an antibiotic to treat my acne? American Academy of Dermatology. Available at: https://www.aad.org/public/diseases/acne/derm-treat/antibiotics (Accessed: 16 March 2024).
- Kim RH, Armstrong AW. Current state of acne treatment: highlighting lasers, photodynamic therapy, and chemical peels. Dermatol Online J. 2011;17(3):2. Published 2011 Mar 15.
- Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003;49(1 Suppl):S1-S37. doi:10.1067/mjd.2003.618
Ask a Dermatologist
Anonymous, fast and secure!

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.

